Pdf view/download
Problem Initial baseline data showed inconsistencies in the glucose management of post-anesthesia care unit (PACU) patients with diabetes mellitus (DM). Some DM patients had their glucose levels monitored and treated while others did not, as treatment was based on anesthesia provider preferences.
Purpose This project aimed to improve postoperative glucose management of patients with DM undergoing surgery by using a glycemic management order set to guide treatment and management of blood glucose levels of diabetic patients in the PACU.
Background This quality initiative was implemented in the PACU at a large level 1 trauma hospital in the Southern United States. The project was conducted to provide an insulin/dextrose protocol so that glucose levels are monitored and abnormal levels are treated appropriately.
Methodology The Plan Do Study Act (PDSA) method of quality improvement was used for this project. Baseline data was reviewed six months before initiating the intervention. Charts of PACU patients with DM were reviewed to see if a glucose check was done, whether abnormal values (<70 mg/dL, >200 mg/dL) were treated, and the time it took to treat abnormal values. A literature review was conducted, and it showed the importance of a protocol in promoting consistent patient care. A glycemic control protocol was developed and implemented. Patient charts were reviewed to assess the effectiveness of the protocol every week for the first three weeks after implementation, then biweekly for the remainder of the implementation period.
Results After 12 weeks of implementation, the data showed that while 100% of diabetic PACU patients received a glucose check upon admission to the PACU, only 80% had the glycemic protocol ordered, meaning that abnormal glucose levels may not have been treated or not treated in a timely manner. However, all DM patients with the glycemic protocol in their order set were treated appropriately per the protocol within 30 minutes of admission.
Implications The presence of a glucose control protocol improved treatment of abnormal glucose levels for DM patients in the PACU.
Introduction
The Centers for Disease Control and Prevention (CDC) estimates that 11.3% of the US population, a total of 37.3 million people, have diabetes (CDC, n.d.-a). Diabetes mellitus (DM) is a chronic disease that affects the body’s ability to make or utilize insulin to help cells use blood glucose to create energy (CDC, n.d.-b). Surgery can cause metabolic stress in DM patients, causing them to be more susceptible to infection and poor glycemic control (Dhatariya et al., 2012). Poor glycemic control can lead to surgical site infections, postoperative morbidity and mortality, and increased healthcare costs (Al-Niaimi et al., 2014).
Anesthesia teams place post-anesthesia care unit (PACU) orders that guide the postoperative management of diabetic patients. Studies have shown that the presence of a glycemic monitoring and control protocol improves the management of patients with DM (Jinjing et al., 2021). Appropriate management and monitoring of DM patients in the PACU is key to safe recovery (Li et al., 2020).
Problem
Initial baseline data on postoperative DM patients in the PACU at a level 1 trauma center identified inconsistencies in the monitoring and management of their glucose levels. Some DM patients had their glucose levels monitored and abnormal values treated while others did not, and treatment was based on anesthesia provider preferences.
Purpose
The purpose of the PACU Glycemic Control (PGC) project was to improve management of diabetic patients in the postoperative PACU area by creating a systematic approach to glycemic control in order to decrease postoperative complications.
Specific Aim
The implementation of the PGC initiative will improve glucose management of DM patients in the PACU so that within three months of implementation, greater than 80% of diabetic patients will receive a point-of-care (POC) glucose check and treatment (insulin or dextrose) when necessary within 30 minutes of PACU admission.
Background
In the past 50 years, there has been an increase in DM around the world. The incidence of DM is expected to rise from 171 million in 2000 to 350 million in 2030 (Basha et al., 2019). To prepare for planned surgery, patients are required to avoid eating for an average of 8 hours. Studies agree that glucose management is critical during the surgical period in patients with DM, as fasting requirements and the stress of surgery place DM patients at high risk for poorly controlled glucose levels (Basha et al., 2019; Al-Niaimi et al, 2014; Godoy et al., 2012; Jinjing et al., 2021; Joshi et al., 2010; Keegan et al., 2010; LaBoone et al., 2014; Sudhakaran & Surani, 2015; Vogt & Bally, 2020), which is a major factor in postoperative morbidity and mortality (Dhatariya et al., 2012). These patients are also at risk for surgical site infections that can result in increased length of stay and increased healthcare costs (Al-Niaimi et al., 2014). Perioperative hyperglycemia is also associated with increased arrhythmias and ventilator dependence (Sathya et al., 2013).
Keegan et al. (2010) and Jinjing et al. (2021) both recommend the use of an insulin protocol to improve postoperative glucose management. Surgical complications and episodes of hyperglycemia and hypoglycemia can be decreased by the implementation of glucose control strategies during perioperative care (Basha et al., 2019; Dhatariya et al.,2012; Godoy et al., 2012; Jinjing et al., 2021; Sathya et al., 2013; Sudhakaran & Surani, 2015; Vogt & Bally, 2020). Usage of these strategies also leads to a decrease in mortality and morbidity rates, length of hospital stay, and the occurrence of prolonged surgical healing time. Having clinical practice guidelines in place promotes the implementation of glucose management strategies, and electronic medical record (EMR) reminders increase adherence to evidence-based guidelines by up to 84.5% (Li et al., 2020).
Perioperative Glucose Management
Evidence shows that healthcare providers should aim to maintain glucose homeostasis during the perioperative period (Basha et al., 2019; Dhatariya et al.,2012; Godoy et al., 2012; Jinjing et al., 2021; Sathya et al., 2013; Sudhakaran & Surani, 2015; and Vogt & Bally, 2020). Glucose management in the perioperative phase entails care given by a variety of providers including preoperative nurses, anesthesia team, surgical team, and postoperative nurses. This can lead to a lack of uniformity in care and increase the risk of error.
Findings suggest that the use of a glycemic protocol is more effective than allowing providers to care for DM patients however they choose (Li et al., 2020). Implementing a protocol at this institution was feasible, as the PACU nurses already receive orders to check patient glucose levels immediately after surgery. However, there were no standing orders to treat abnormal values. After checking the patient’s glucose level, the nurse had to contact an anesthesia provider to receive additional orders to treat values <70 mg/dL or >200 mg/dL. The establishment of a standard glycemic control protocol would allow nurses to have orders in hand to treat patients with abnormal glucose values, and the inclusion of a notification in the EMR would remind the PACU nurses of the patient’s last dose of insulin in the operating room (OR), decreasing the risk that patients may receive multiple doses of insulin. The cost to implement the change was minimal, as no new equipment or staff were required.
Methods
Context
The project was implemented at a level 1 trauma center in the Southern United States. The institution has 23 main ORs, six ambulatory ORs, and many other procedural areas. The anesthesia department provides care in all these areas. The anesthesia team is made up of about 70 certified registered nurse anesthetists (CRNAs), 100 resident physician anesthesiologists, and 60 physician anesthesiologists. In 2021, the institution conducted 19,989 surgical procedures, 575,109 radiology procedures, and over 13 million pathology procedures. This initiative was implemented in the PACU that services the 23 main ORs.
Improvement Team
The quality improvement team included the CRNA project manager, an anesthesiologist, a pharmacist, the PACU nurse manager, and a data analyst.
Project Methodology
The Plan Do Study Act (PDSA) methodology was used to develop, implement, and evaluate the PACU Glycemic Control (PGC) initiative. There was a 3-month implementation period.
Intervention
Evaluation of the anesthesia provider-initiated management plan for diabetic postoperative patients identified a number of issues. The anesthesia team was responsible for management of diabetic PACU patients until they were either discharged home or sent to a different unit. A chart review revealed inconsistencies in the monitoring of patients with DM in the PACU. While the anesthesia team used an existing order set to specify PACU orders, the order set did not include indications to treat abnormal glucose levels. When PACU nurses paged or called anesthesia providers requesting an order to treat glycemic levels >200 mg/dL or <70 mg/dL, providers did not always respond promptly or chose not to treat abnormal values. Additionally, PACU nurses were unaware of what intraoperative medications were given to manage a patient’s blood glucose and did not have an order to repeat the POC glucose test as needed.
Implementation Plan
The improvement team outlined ideas to improve glucose management that included revising the anesthesia-initiated PACU order set to incorporate a glycemic control protocol that would create uniformity in the care of postoperative DM patients. The implementation plan consisted of:
- Development of a glycemic control protocol
- Approval of the protocol by the anesthesia, information technology (IT), PACU, and pharmacy teams
- Integrating the glycemic control protocol into the PACU order set
- Embedding a notification process in the EMR to inform the PACU nurses of the patient’s last insulin dose
- Introducing a PowerPoint education/ training module for PACU nurses regarding the new glycemic control order set and how to interpret it
- Instructing CRNAs on how to order the glycemic control protocol
- Notifying anesthesiologists via email about the changes to the order set and the importance of using the new order set for diabetic surgery patients
Development of the Glucose Control Protocol
Glucose management practice pre-intervention required PACU nurses to perform POC glucose level tests on diabetic PACU patients and then notify the anesthesia provider if patient values were <70 mg/dL or >200 mg/dL. The anesthesia provider would then decide whether and how to treat the abnormal glucose value. Review of current practice revealed inconsistencies in the care provided. Figure 1 and Figure 2 describe the original PACU glucose management practice and the changes made with the introduction of the glycemic control protocol. According to the protocol, the anesthesia provider is responsible for writing the glycemic control PACU orders for diabetic patients upon completion of the surgical case by checking a box in the EMR. There are two order set options: one order set for patients who weigh less than 80 kg and another for patients who weigh 80 kg or more. When the patient arrives in the post-anesthesia care unit, the PACU nurse reviews the order set, checks the patient’s glucose level, and treats abnormal values (<70 mg/dL or >200 mg/dL) as per the protocol.
The project implementation team modified the glycemic protocol used by the anesthesia team in the operating room, creating one that was more conducive to preventing hypoglycemic episodes in the PACU due to insulin overdose. The new PACU glycemic protocol stipulates that POC glucose checks should be performed every hour while the DM patient is in the PACU and specifies how much insulin should be administered to treat hyperglycemia (blood glucose level >200 mg/dL) based on patient weight, cautioning that patients should not be re-dosed with insulin within four hours of their previous dose. PACU nurses are required to notify an anesthesia provider if patients become hypoglycemic as indicated by a glucose level <70 mg/dL. The protocol states that hypoglycemic patients are treated with dextrose, and a POC glucose check should be performed 30 minutes after administering the dextrose.


Staff Education
Prior to implementing the glycemic management order set, the anesthesia providers were instructed on how to place the new PACU order set. In turn, PACU nurses received education on the details of the glycemic control protocol.
Measures
The desired outcome of the PACU Glycemic Control initiative was to improve glucose management of diabetic patients in the PACU so that greater than 80% of DM patients receive a POC glucose check and treatment of abnormal values is initiated within 30 minutes of PACU admission.
Process Measures
- The percentage of DM patients with glycemic control orders. This was calculated by comparing the number of DM patients in the PACU with glycemic control orders to the total number of DM patients in the PACU. There were 108 patient charts reviewed and analyzed. Providers who did not order the glycemic protocol received an email with information on how to order the protocol and were reminded to utilize the new order set.
- The percentage of DM patients receiving POC glucose checks in the PACU. This was determined by comparing the number of DM patients with glucose checks to the total number of DM patients in the PACU.
Outcome Measures
- Time to treatment. The percentage of DM patients who were treated appropriately in the PACU. This was determined by the number of patients who received the right treatment versus the total number of DM patients in the PACU. Appropriate treatment was defined as the correct amount of insulin or dextrose administered as dictated by the protocol.
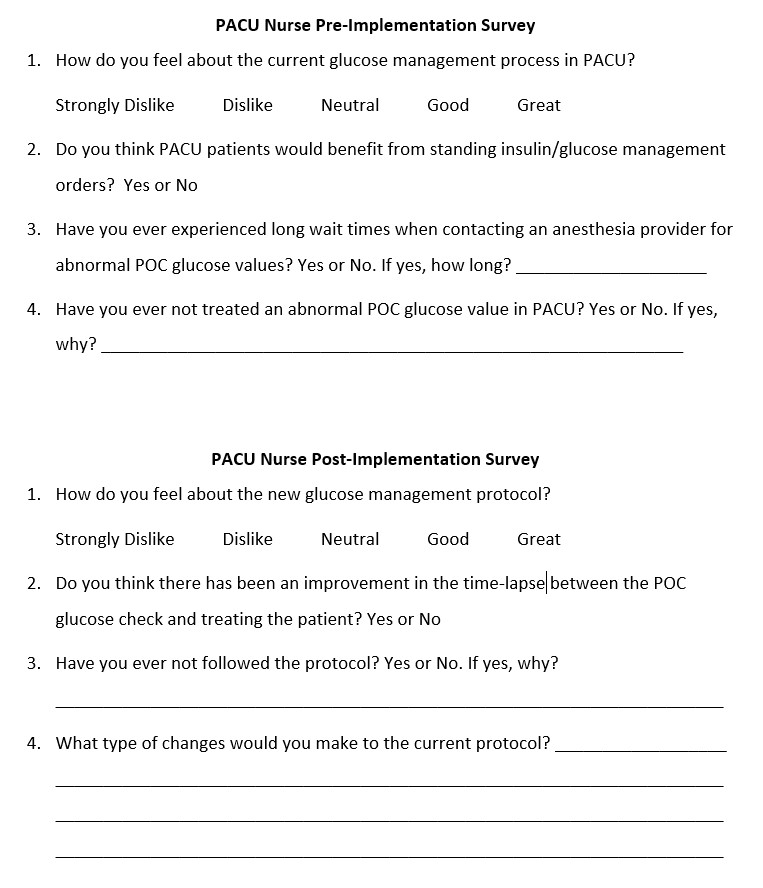
- PACU nurse satisfaction level. PACU nurses completed a pre- and post-implementation survey to inform the project implementation team regarding the adjustment of the PACU nurses to the new order set and their satisfaction with the glycemic control protocol (Appendix A). The goal was to have at least 80% of PACU nurses express satisfaction with the protocol.
Data Analysis
The data required to examine the project measures were obtained by auditing patient charts every week for the first three weeks after implementing the intervention, followed by biweekly audits for the remainder of the implementation period. Data was collected with the help of a data specialist and the “SlicerDicer” component in the Epic EMR. The SlicerDicer allows a search for patient charts based on criteria entered. The criteria used to collect the data included anesthesia records, presence of diabetes, admission to the PACU, and date. Cases where patients were sent back to the medical-surgical floor or intensive care unit post-surgery or had procedures outside the operating room were excluded. The implementation team reviewed the charts of all DM patients in the PACU on the busiest day of the week for the OR (Thursday); there was an average of 10 patients with each audit, resulting in a total of 108 chart audits.
Data were analyzed using descriptive statistics to compare baseline data with outcome data collected at each audit. Members of the implementation team reviewed audit results. Based on the findings as well as on feedback from the PACU nurses and anesthesia team, they either reminded caregivers to follow the project’s intervention process or adjusted the process and/or the protocol itself. The effectiveness of the PGC initiative was assessed by determining to what degree DM patients in the PACU received glycemic protocol orders, had a POC glucose level check upon PACU admission, and, where indicated, were treated with insulin or dextrose per the protocol within 30 minutes of admission. To evaluate PACU nurse satisfaction with the new protocol, the implementation team conducted a comparison between the pre- and post-implementation surveys completed by the nurses.
Ethical Considerations
The institution’s Quality Assurance Improvement Committee (QAIC) approved the implementation of a glucose control protocol. The Institutional Review Board (IRB) concluded that the project did not meet the regulatory definition of human subject research and therefore did not require their oversight. All data management adhered to Health Insurance Portability and Accountability Act (HIPAA) laws. Data was collected from a password-protected EMR, and all data was de-identified and stored in a locked database.
There were no known conflicts of interest with this project. None of the key personnel have disclosed affiliation with pharmaceutical companies producing or distributing insulin or dextrose.
Results
Glycemic Control Protocol Outcomes
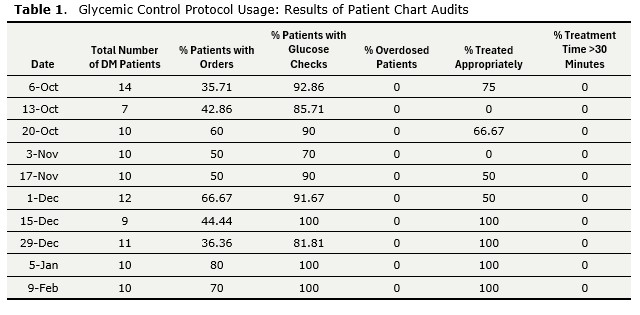
Baseline data showed that 22 DM patients received care in the PACU, two patients had abnormal values (9%), one of those two patients was treated (50%), and seven patients did not have a POC glucose check (32%). At the beginning of the implementation phase, data showed only 35.7% of patients with DM had the glycemic protocol ordered. Two weeks later, the protocol was present on 60% of the DM patient charts and 90% of diabetic patients received POC glucose checks (Figure 3 and Figure 4).
For two months after implementation of the glycemic protocol, the anesthesia providers used the order set consistently until the end-of-year holiday season, when the glycemic protocol orders for DM patients dropped drastically. The percentage of patients with glycemic orders decreased to 36.4%, and the percentage of patients receiving POC glucose checks dropped to 81.8% (Figure 3 and Figure 4). The numbers suggested that a change in anesthesia providers during the holiday period negatively impacted the awareness and consistent use of the intervention. In addition, there was limited communication from the implementation team related to the project during that time. An email was sent out at the end of the holiday season to remind providers of the ongoing project. Consequently, there was an increase in compliance with using the order set at the start of the new year.


Table 1 describes the results of each of the patient chart audits. By the end of the 3-month implementation period, all of the desired outcome goals were met or exceeded; 80% of the PACU patients with DM had glycemic protocol orders, 100% of the patients received POC glucose checks, all patients with abnormal glucose levels were treated appropriately per the glycemic protocol within 30 minutes of admission to the PACU, and no patients were overdosed with insulin. However, when data was collected a month later, it was noted that compliance in ordering the glycemic control protocol had dropped from 80% to 70% (Table 1).
Nurse Satisfaction
A baseline survey of 12 PACU nurses identified that 30% (n=4) reported delays in treating abnormal glucose values, and 70% (n=8) stated that they did not treat abnormal glucose values because the anesthesia provider either did not call back or chose not to treat the patient. A post-implementation survey of PACU nurses (n=12) reported no delays in treating abnormal values. However, 30% (n=4) commented that there were times when they needed to remind an anesthesia provider to order the glycemic control protocol.
A comparison of pre- and post-implementation survey results showed that the number of PACU nurses who felt good or great about management of DM patients in the PACU increased from 50% to 83%. 17% of nurses (n=2) who did not feel good or great about the new process identified that the glycemic control protocol was not ordered universally for all DM patients admitted to the PACU.
Discussion
Summary of Outcomes
The implementation of the PACU Glycemic Control project showed an improvement in the monitoring and treatment of DM patients in the PACU. There were periods of inconsistency that improved upon increased communication with anesthesia providers. The addition of the PACU glycemic control protocol aligned with the literature that suggests that the presence of a glycemic protocol improves the management of DM patients in the postoperative area (Keegan et al., 2010; Jinjing et al., 2021). The protocol enabled PACU nurses to treat patients for abnormal glucose levels without having to contact an anesthesia provider, leading to a greater percentage of patients being treated appropriately and quickly.
The project’s Aim Statement sought to ensure that within three months of the addition of a glycemic control protocol to PACU orders, 80% of PACU patients who have DM will be monitored via POC glucose checks and, if necessary, treated for abnormal glucose levels within 30 minutes of admission to the PACU. This goal was achieved. Upon completion of the 3-month intervention period, 80% of diabetic patients were admitted to the PACU with glycemic control orders, a 44% improvement over baseline data;100% of DM patients received a POC glucose check upon admission, and 100% of patients with abnormal glucose levels (<70 mg/dL or >200 mg/dL) were accurately treated per the protocol within half an hour (Table 1). The decision to modify the existing glycemic protocol used by the anesthesia team in the operating room to incorporate measures to prevent insulin overdose in the PACU proved to be effective; no episodes of overdosing were reported for the implementation period (Table 1).
Strengths of the Initiative
The strengths of the PGC initiative included a multidisciplinary implementation team, the receptiveness of the PACU nurses to the new protocol, and the affordability of the project. The multidisciplinary team members each lent their expertise to the project, providing for effective implementation. While PACU nurses expressed some concern over having to remind anesthesia providers to place glycemic control orders for DM patients, they viewed the protocol as a benefit to the patients and accepted the change with enthusiasm. From a budgetary perspective, the implementation of the glycemic control protocol did not require any out-of-pocket expenses for the institution, as it streamlined an already existing process.
Challenges Faced
Evaluation of the outcomes of the PACU Glycemic Control initiative identified a decrease in ordering the protocol at the beginning of the second and third months of the implementation period. The institution is a teaching hospital, and a new group of anesthesia residents rotates through the OR at the beginning of every month. New providers unaware of the protocol could explain the lack of consistency in ordering the protocol. Another contributing factor was that the anesthesia team hired new CRNA locums during the implementation phase. The rotating residents and new CRNAs were initially unaware of the PGC initiative and had to be reminded to place the protocol order, emphasizing the fact that communication is key to the success of a QI project.
At this institution, the average time spent by a patient in the PACU is about 45 minutes, which is not enough time to adequately assess the effects of treating abnormal blood glucose levels. Therefore, the argument that 100% of patients experiencing hypo- or hyperglycemia were treated appropriately is based solely on whether the protocol’s treatment indications were followed and not on the effectiveness of treatment.
Barriers to successful project implementation included a delay in initiating the intervention and poor communication with temporary anesthesia staff filling in during the holiday season about using the new order set to include the glycemic control protocol. There was a 2-month launch delay related to the need for an information technology (IT) specialist to add the protocol order set to the EMR that was needed to coincide with institution-wide updates to the Epic system. Compliance with the intervention was hindered during the one-month holiday period (December) due to a failure to communicate the new process to anesthesia providers staffing the OR during the holidays.
Upon the introduction of the diabetic management protocol by the QI team, some anesthesia providers were indifferent to the project and did not use the new order set. PACU nurses reported that some diabetic patients experiencing hypoglycemia or hyperglycemia were not treated appropriately because anesthesia providers did not agree that the patient’s glucose levels needed management. Some providers felt that patients with hyperglycemia in the postoperative area did not need to be treated because they do not eat while recovering in the PACU. This may have contributed to the slow start in ordering the protocol at the beginning of implementation.
One month post-implementation, an audit of patient charts revealed that compliance with the PGC intervention was still well below 80% (Table 1). In response, the implementation team emailed reminders to anesthesia providers whose DM patients did not have glycemic control protocol orders when admitted to the PACU or were not treated appropriately per the protocol. This was repeated at the end of month 3 of implementation. Both reminder emails were followed by increases in the percentage of DM patients with the new order set.
Sustainability
Both the anesthesia providers and PACU nurses found that the new protocol streamlined the care of diabetic patients in the postoperative period. The diabetic management order set became an expected care management process for diabetic patients in the PACU. It is important to note that as the project progressed, the PACU nurses took the initiative to ask anesthesia providers to order the protocol whenever they noticed that glycemic control orders had not been placed for PACU patients who were diabetic or needed glucose management.
The outcome data that identified the inconsistent use of the new protocol underscored the need for the order set to be hardwired within the EMR, as changes in care providers or reliance on memory alone can negatively impact effective, consistent use of a process that is only partially automated. A reasonable next step for the PGC initiative is to add a feature to the EMR that automatically initiates the glycemic control protocol when the POC glucose check is ordered for diabetic PACU patients.
Conclusions
The addition of a glycemic control protocol to the PACU orders at this institution created an opportunity to simplify the management of DM patients post-surgery. The protocol enabled PACU nurses to assess and treat abnormal blood glucose values without having to contact an anesthesia provider, resulting in uniform and timely treatment while also preventing insulin overdose.
References
Al-Niaimi, A. N., Ahmed, M., Burish, N., Chackmakchy, S. A., Seo, S., Rose, S., Hartenbach, E., Kushner, D. M., Safdar, N., Rice, L., & Connor, J. (2014). Intensive postoperative glucose control reduces the surgical site infection rates in gynecologic oncology patients. Gynecologic Oncology, 136(1), 71–76 https://doi.org/10.1016/j.ygyno.2014.09.013
Basha, A.A., Vivekanandan, S., & Parthasarathy, P. (2019). Blood glucose regulation for postoperative patients with diabetes and hypertension continuum: A cascade control based approach. Journal of Medical Systems, 43(4), 1–8. https://doi.org/10.1007/s10916-019-1224-6
Centers for Disease Control and Prevention (CDC). (n.d.-a) National Diabetes Statistics Report. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed 3.16.2023
Centers for Disease Control and Prevention (CDC). (n.d.-b) Diabetes Basics. https://www.cdc.gov/diabetes/about/index.html#cdc_disease_basics_overview-overview. Accessed 3.16.2023
Dhatariya, K., Levy, N., Kilvert, A., Watson, B., Cousins, D., Flanagan, D., Hilton, L., Jairam, C., Leyden, K., Lipp, A., Lobo, D., Sinclair-Hammersley, M., Rayman, G., Joint British Diabetes Societies (2012). NHS diabetes guideline for the perioperative management of the adult patient with diabetes. Diabetic Medicine, 29, 420-33. https://dx.doi.org/10.1111/j.1464-5491.2012.03582.x
Godoy, D. A., Di Napoli, M., Biestro, A., & Lenhardt, R. (2012). Perioperative glucose control in neurosurgical patients. Anesthesiology Research and Practice, 2012, 1–13. https://doi.org/10.1155/2012/690362
Jinjing, W., Kang, C., Xufei, L., Xueqiong, L., Xinye, J., Miao, Y., Jinping, Z., Zhaohui, L., Jingtao, D., Yaolong, C., Linong, J., & Yiming, M. (2021). Chinese clinical practice guidelines for Perioperative Blood Glucose Management. Diabetes/Metabolism Research and Reviews, 37(7). https://doi.org/10.1002/dmrr.3439
Joshi, G. P., Chung, F., Vann, M. A., Ahmad, S., Gan, T. J., Goulson, D. T., Merrill, D. G., & Twersky, R. (2010). Society for Ambulatory Anesthesia Consensus Statement on perioperative blood glucose management in diabetic patients undergoing ambulatory surgery. Anesthesia & Analgesia, 111(6), 1378–1387. https://doi.org/10.1213/ane.0b013e3181f9c288
Keegan, M. T., Vrchota, J. M., Haala, P. M., & Timm, J. V. (2010). Safety and effectiveness of intensive insulin protocol use in post-operative liver transplant recipients. Transplantation Proceedings, 42(7), 2617–2624. https://doi.org/10.1016/j.transproceed.2010.05.156
LaBoone, L. M., McLarney, J. T., & Reynolds, L. R. (2014). An interdepartmental collaboration to improve preoperative glycemic control. Hospital Practice, 42(5), 83–88. https://doi.org/10.3810/hp.2014.12.1161
Li, G., Dietz, C. J., Freundlich, R. E., Shotwell, M. S., & Wanderer, J. P. (2020). The impact of an intraoperative clinical decision support tool to optimize perioperative glycemic management. Journal of Medical Systems, 44(10). https://doi.org/10.1007/s10916-020-01643-1
Sathya, B., Davis, R., Taveira, T., Whitlatch, H., Wu, W. (2013). Intensity of peri-operative glycemic control and postoperative outcomes in patients with diabetes: a meta analysis. Diabetes Research and Clinical Practice., 102(1), 8–15. https://dx.doi.org/10.10.16/j.diabres.2013.05.003
Sudhakaran, S., & Surani, S. R. (2015). Guidelines for perioperative management of the Diabetic patient. Surgery Research and Practice, 2015, 1–8. https://doi.org/10.1155/2015/284063
Vogt, A. P., & Bally, L. (2020). Perioperative glucose management: Current status and future directions. Best Practice & Research Clinical Anaesthesiology, 34(2), 213–224. https://doi.org/10.1016/j.bpa.2020.04.015.
Article Information
Author Affiliations
Cizik School of Nursing
University of Texas Health Science Center at Houston
Houston, Texas
Corresponding Author
Chinwe C. Ononogbu
Cizik School of Nursing
University of Texas Health Science Center at Houston
6901 Bertner Ave
Houston, TX 77030
DOI: 10.26051/d-rvam-pg0z
Appendix A